Latest
-

Symposium: Reversing Chronic Diseases Healing and Calibrating Environments
Reversing Chronic Diseases: Healing and Calibrating Environments The United States has an enormous burden of chronic diseases that continues to challenge the healthcare system. An estimated sixty percent of Americans live with at least one chronic disease. The symposium “Reversing Chronic Diseases: Healing and Recalibrating Environments” outlines an approach to understanding and healing from chronic…
-
Love is a Listening Practice
One of the greatest gifts we can give ourselves is to develop a practice of self-love. Love flourishes by building skills to support the nervous system even in the setting of challenge and uncertainty. The practice creates greater resilience for short- and long-term goals and connects us with our purpose. Love is the meeting place…
-

Love is a Healing Practice
Love is the greatest skill we can build for our health and life. -it is developing a sense of what defines you and how you wish to define yourself – a meeting of loving acceptance and loving growth – one that comes with challenge, discomfort, and change – to develop an adaptation that creates greater…
-
The Harmful Impact of Shame on Health: Understanding and Overcoming Its Effects
Shame is a complex, often overwhelming emotion that has deep roots in our personal experiences, cultural background, and self-perception. Unlike guilt, a feeling associated with regret for a specific action, shame is a sense of inadequacy or worthlessness that often permeates one’s sense of self. It is a powerful force that can lead to a…
-

AI-Powered Tools: Revolutionizing Mental Health Care
Integrating Artificial Intelligence (AI) into healthcare has revolutionized various medical fields, from diagnostics to treatment planning, offering unprecedented advancements in accuracy, efficiency, and accessibility. Among these transformative areas, clinical psychology and mental health have become increasingly fertile grounds for AI applications. With mental health issues on the rise globally—exacerbated by the complexities of modern life,…
-

Understanding Weight Plateaus: Practical Solutions
by Julian Dollente, RN and Christopher M. Cirino, DO, MPH Embarking on a wellness journey can be a transformative experience. It involves commitment, consistency, and a willingness to adapt and grow. One of the most frustrating challenges many encounters is hitting a weight plateau. This occurs when one’s progress stalls despite continued efforts with diet…
-

10 Proven Ways to Boost Motivation and Achieve Your Goals
“The only limit to our realization of tomorrow will be our doubts of today. “ – Franklin D. Roosevelt Motivation is the driving force that propels us towards our goals and aspirations. Whether you’re striving for personal growth, pursuing a career change, or working on a creative project, it’s essential to maintain high levels of…
-

How Can a Healthy Diet Prevent Dementia?
In an aging world, dementia has emerged as a pressing concern, casting a shadow on the lives of millions of individuals and their families. It robs them of their cognitive abilities, memories, and independence. There are currently more than 55 million people globally with dementia, with nearly 10 million new cases every year. Alzheimer’s disease…
-
Making Healthy Food Choices: Processed vs Natural Food
Introduction by Hanna Keith Santos Barrientos Nutrition is a crucial element in achieving a healthy lifestyle. However, with most food products being advertised as healthy and nutritious, one may wonder if they’re making the right food choices. If you’re someone who wants to lead a nutritious diet, you can start by understanding the difference between…
-

Stress Management: How to Overcome Stress and Turn It Into Healthy Practices
“The greatest weapon against stress is our ability to choose one thought over the other.” — William James The adage “your thoughts, not the situation” bears truth when discussing stress. Indeed, stress is a natural and unavoidable part of life; it is our body’s automatic response to the challenges and adversities we encounter every day.…
-

The Health Impacts of Stress
Not everyone is affected similarly by the same stressor. Stress is both Stressor and Stress Reaction. I hear a lot of times in the clinic how an individual was doing fine until another person or an unfortunate circumstance contributed to their increased stress, anger, and pain. We cannot live a stress-free life. When we speak…
-

Women’s Health: Understanding the Natural Changes That Come With Aging
By Hanna Keith Santos Barrientos edited by Christopher Cirino, DO, MPH Here is an article specific to women’s health: menopause and the hormonal changes of aging. It also discusses how older women can maintain a healthy body and be able to adapt to the changes that come with aging. As women, our bodies have constantly…
-
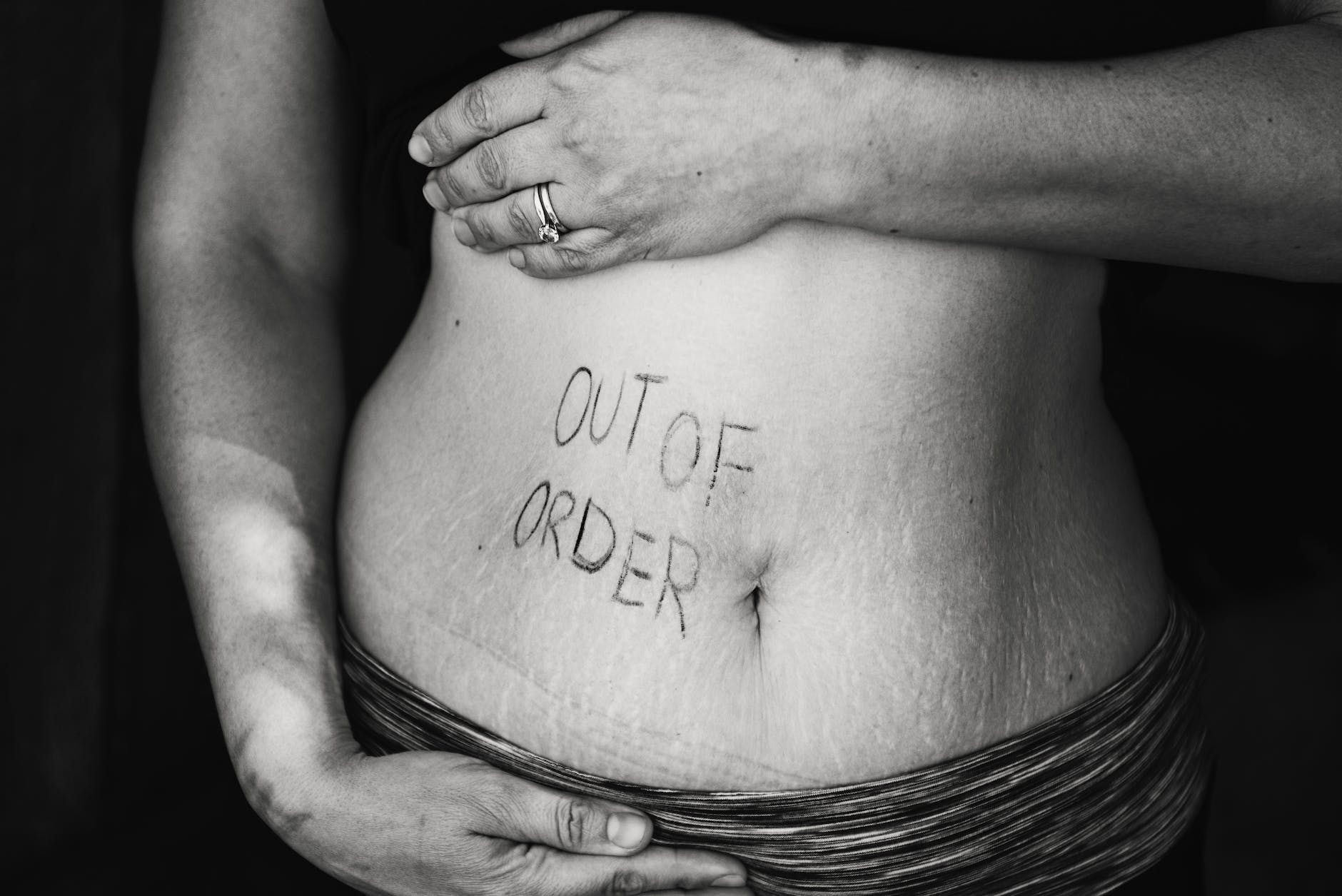
Exocrine Pancreatic Insufficiency and Diabetes: What You Need to Know
Do you have diabetes mellitus? Exocrine pancreatic insufficiency is an important condition which also affects the pancreas and can have significant health impacts. You may be surprised that it affects up to 50% of people with diabetes. And EPI is a condition that could go unnoticed or misattributed without actively screening for it. Exocrine Pancreatic…
-

Is Psilocybin a Promising New Therapy for Depression?
A lot has happened these past few years that may have contributed to people’s anxiety and depression more than ever. In fact, about 16 million American adults experience depression every year. Modern medicine has come a long way with the help of research and technology, but typical antidepressants may not be as effective in dealing…
-

Is Dementia Preventable and Reversible?
Introduction: Definition of Alzheimer’s Dementia Alzheimer’s disease is the most common type of dementia. The characteristic findings for Alzheimer’s are amyloid plaques and neurofibrillary tangles. Amyloid plaques occur due to abnormally high levels of beta-amyloid, a protein indicative of disease progression. Beta-amyloid is a naturally occurring protein found between neurons in the brain, but it…
-

Cervical Cancer: A Call for Prevention
Cervical cancer is the fourth most common cancer affecting women worldwide, and it is the leading cause of cancer-related deaths in women. The WHO projects that the number of cases will increase from 570,000 to 700,000 annually between 2018 and 2030. Along with these increases comes deaths, expected to increase from 311,000 to 400,000 annually. Women…
-

The Evolution of the Approach to Mental Health: Towards a More Preventive Strategy
The pandemic has given us a lot to think about regarding mental health. Already on an incline, the rates of depression and anxiety have increased over the last few years. Psychiatry is on the reactive side of mental health, addressing issues as people present with more serious conditions. The ACEs study showed an association of…
-

Posttraumatic Stress Disorder and the Rise of Chronic Diseases
I have worked in a prison for the last seven months. Nearly everyone who I have seen for clinic visits has reported some degree of trauma in their childhood. Studies corroborate this and show that 90% of juveniles committing crimes have a history of childhood trauma. The crucial and poignant message is that past trauma…
-

Is it Possible to Reverse Thyroid Disease?
As much as 90% of thyroid diseases are autoimmune (AITD). Hashimoto’s Thyroiditis (HT) is the most common cause of thyroid disorder and affects about 1 in 50 people in the US. It is an autoimmune disease caused when a particular white cell (lymphocytes) invades the thyroid tissue. The cells cause tissue inflammation and thyroid dysfunction, which is gradually replaced…
-

Your Sex Life: 10 Reasons Why You Should Improve It
How has your sex life been? Are you having enough? These questions might be too taboo for some people. But you should know that sex is natural, and we all need it. Sex is an integral part of human life and is beneficial to our overall well-being. Some argue that sex should fall under basic…
-

Does Exercise Improve Mental Health?
From an early age, we are taught how regular exercise can positively impact our bodies, increase our muscle mass, lower our blood pressure, boost our energy, minimize our risk of disease, and improve practically every aspect of our physical health. But what about other aspects, such as mental health? Aside from physical benefits, having a…
-

Hypothyroidism: 7 Associated Conditions to Know About
by Christopher M. Cirino DO, MPH and Julian Dollente, RN The Most Common Cause of Hypothyroidism is Autoimmune For those of you who have hypothyroidism, which is about 5% of the US population, you will find this article useful. An autoimmune cause of thyroid dysfunction accounts for 90% of hypothyroidism. Knowing that your hypothyroidism has…
-

The Most Common Thyroid Disease: A Deeper Look
by Christopher M. Cirino, DO MPH and Julian Dollente, RN. The endocrine systems consist of multiple tissues, organs, and glands distributed throughout the body. It interacts with the immune system. While the body employs the immune system to protect from foreign invaders, it sometimes attacks the body’s cells, such as your thyroid gland. Hashimoto’s is…
-

Got Acid? GERD and Its Less Common Presentations
Have you ever had a feeling of burning pain in your chest or throat after having a delicious meal? How about having a sour or bitter taste up into your throat or mouth? If you have, you are not alone. These are the typical symptoms of acid reflux, a normal condition when experienced occasionally. Acid…
-

Does Marijuana Kill Brain Cells?
by Ayotola Ogunsipe, edited by Christopher M. Cirino, DO MPH As of 2021, marijuana is currently legal in eighteen of the United States; 15 additional states have decriminalized use. It appears that the bad reputation it has garnered over the years is gradually diminishing. The renewed interest comes amid marijuana’s possible benefits in chronic pain,…
-

Is Coffee Harmful to Your Health?
Is Coffee Harmful to Your Health? A Daily Apple on the Effects of Caffeine in Coffee and other foods. There’s something incredibly soothing about waking up to the smell of freshly brewed coffee. However, millions of coffee drinkers don’t just take their cup of joe daily because of its aroma; it’s also a delight because…
-

Tending the Garden Within: Does Meditation Reverse Aging?
by Sydney Bright and Christopher Cirino What if as time passes, our bodies did not age? Does growing older always have to lead to a sharp decline in physical health? Is it possible to live long with a vibrant, healthy body? Modern science is beginning to challenge our preconceived notions of aging, and the above…
-

The Health Impacts of a Sedentary Lifestyle: Problems and Solutions
The Process of Life Must be Kept in Motion. Dr. Andrew Taylor Still, Founder of Osteopathy We now live in a world where technological advancement has made life easier and more comfortable. Unfortunately, comfort comes with a price. Our modern lifestyles have made it easier to become unhealthy. Over the past several decades, most of…
-

The Gut-Brain Axis and Its Relationship to Health
Introduction to the Gut-Brain Axis Everything is connected. At a large scale, this is true when thinking about our planet: our choices influence our environment, which affects the plants and animals of our ecosystem. Ultimately, the systems come back to influence us once again. These same effects occur locally: the actions and kindnesses we should…
-

Musings on the Brain: Understanding Behaviors
Introduction: Life with a Brain I write an ode to the brain in this article. We live in a world where constant forces require that we must counteract or succumb. We stand against the force of gravity taking us down. We seek shelter from the wind and rain that impose their control over our movement…
-

What are the best non-medical treatments for chronic pain?
What is an evidence-based way to address chronic musculoskeletal pain without medications? Short answer: A Multi-Pronged Approach Including Movement, Stress Management, Low Carbohydrate Diet, Optimal Weight, and Optimal Sleep Introduction: What is the Burden of Chronic Pain? We carry through life the sum-total of trauma to our brains and bodies. As we age, there is…
-

Breast Cancer Screening: What is Recommended?
Breast cancer (BC) has become a global health issue, as it is the leading cause of cancer-related deaths among women worldwide. In 2020 alone, about 2.3 million women were diagnosed with 680,000 deaths worldwide. 7.8 million women received this diagnosis in the past five years, making it the world’s most prevalent cancer. From the 1930s…
-

What is the Best Diet to Lose Weight?
Choosing the best diet for you is a lot like a labyrinth; it’s easy to get lost and sometimes it requires trial-and-error.
-

Fasting: Are There Health Benefits?
Fasting is gaining increasing attention as a potential method to optimize weight and reverse insulin resistance. Can fasting be a helpful practice on the road to optimal health? Here is a quick overview on fasting, types of fasting, and benefits. Early Studies on Mechanism of Fasting We owe much of our knowledge to what happens…
-

The Daily Apple: Best Tips for Good Sleep
This article on sleep was written by Daniela Dominguez, second-year medical student at Universidad Internacional del Ecuador Escuela de Medicina. We all want to wake up and feel refreshed and ready for a new day. One of the keys to a fulfilling life is a goodnight’s sleep. In the past, it was common to think…
-

Erectile Dysfunction: Harder to Get Hard?
There are benefits in reversing chronic disease states that lead to improved functioning in all vascular tissues – including the penis!
-

Menopause: Symptoms and How to Manage It
Every beginning has an end. Menopause is the moment in a woman’s life where ovulation ends. While it may be a natural biological process for a woman, it causes uncomfortable symptoms that disrupt her sleep, lower energy, and affect emotional health. Here is an overview of menopause, including the management of menopausal and perimenopausal symptoms.…
-

What Do Elevated Liver Function Tests Mean?
Let’s say your doctor saw you, and they ran a series of blood tests on you. The bloodwork came back, and your doctor informed you that you had elevated liver function tests. What does this mean? Is there any reason to be concerned about these results? Are Elevated Liver Function Tests any Cause for Concern:…
-

Physician Burnout: 6 Ways to Develop Resilience
The current pandemic has been a catalyst of change in many people. Health guidelines prioritized public safety over other practices, including clinic visits, social activities, worship, and school. Together we waited for the process to pass in our silos, a shared experience in time but not in space. The pandemic also put into the forefront…
-
Sin: How Does Neuroscience Explain It?
As an open flame attracts a moth, an encounter that can end fatally, certain things in life lure us as humans. Whatever one wishes to refer to the attraction of sin, e.g. mistakes, vices or transgressions, does not change their grip on all of us. Is there something intrinsic about being a human that makes…
-

Pandemic Burnout: How Healthcare Professionals Can Cope
Over a year ago, the Covid-19 pandemic broke out and took the entire world by surprise. Although this is not the first outbreak and it will not be the last, modern society hasn’t experienced a health crisis of this nature in decades. Knowing nothing about Covid-19, we led ourselves to believe life could go on…
-

-

The Fractal Whisperer: Musings on health
What is “healthy” and would you know it if you saw it? From nature, we gather our understanding of life and how our environment affects us. We develop insights or “laws” – of gravity, entropy and heavenly bodies, through the observations we make in the world around us. At its essence, a law is a…
-

MRSA Infections: Best Advice for Treating and Preventing Them
The article is a summary on treating MRSA and other Staph aureus skin infections and colonization. If you have had Staph aureus infections, this article is a great way to prevent further problems with this bacteria. As an infection doctor, this is one of the most common reasons that I see people. This article is packed with information. If…
-
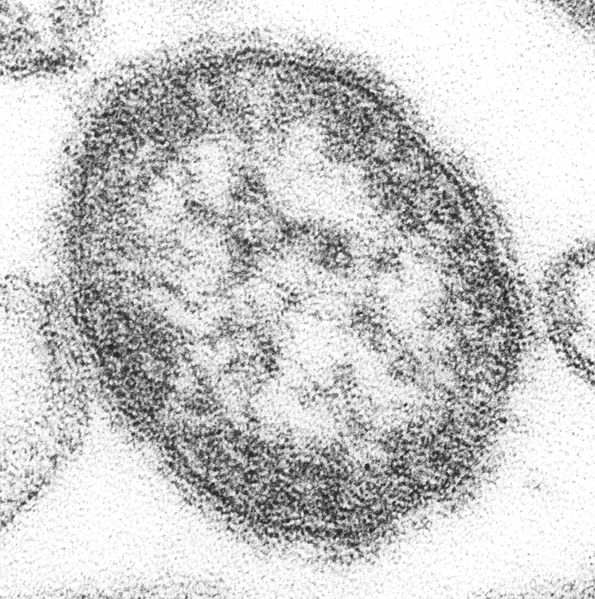
8 Questions and Answers for the Measles Outbreak NW
Update 2/28/2019: As of today, there have been 65 confirmed and 4 suspected cases of measles in Clark county , Washington; 57 of the cases were in those unvaccinated; 6 cases with unverified vaccine status. The majority (47) of cases were in children 11 and under. There was 1 confirmed case of measles in King…




